As we approach 2026, the world of medical coding is experiencing a significant shift. This period is arguably one of the most consequential in recent memory. Changes in regulations, the demands of payers, evolving documentation standards, and the increasing influence of technology are all converging to redefine how medical practices handle service reporting, revenue capture, and compliance.
For those in the healthcare field—providers, coders, billers, and practice managers—keeping up with the latest information is now a necessity. A single misstep in coding updates can trigger claim denials, slow down payments, invite audits, or create compliance issues, all of which can impact a practice’s bottom line.
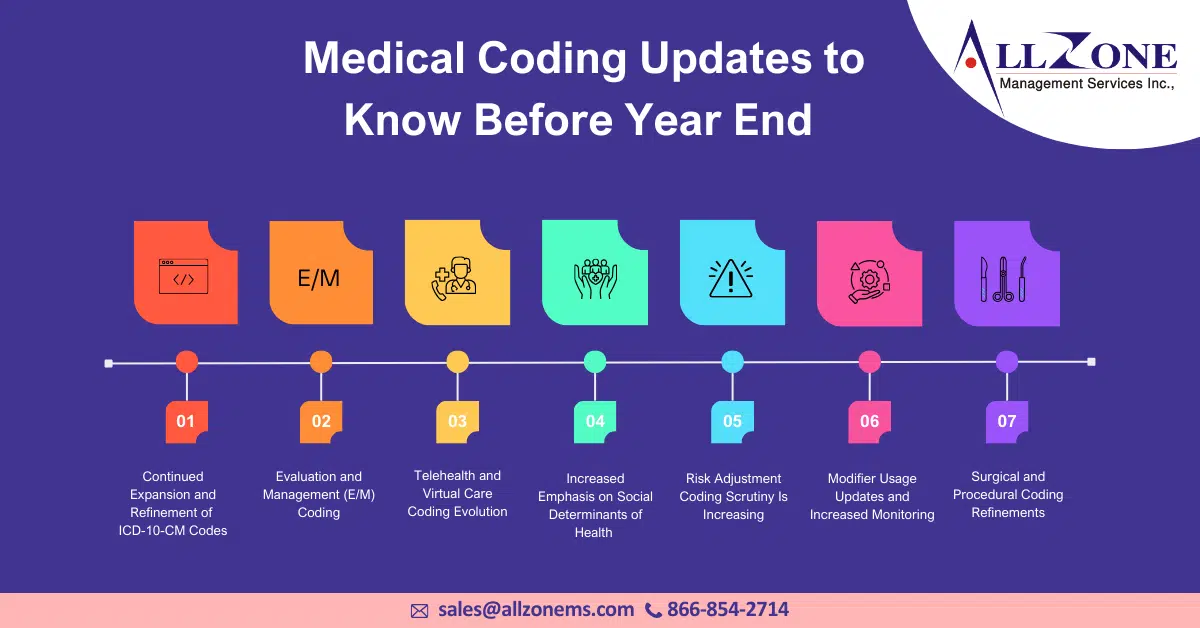
This newsletter highlights the essential medical coding changes that every practice needs to understand before 2026. We’ve broken them down in a straightforward, practical way, avoiding unnecessary technical language. If you’re a solo practitioner, part of a multi-specialty group, or work in revenue cycle management, these updates will affect how you code, bill, and document patient care in the future.
Why Medical Coding Updates Matter More Than Ever
Medical coding is the backbone of healthcare reimbursement. Every CPT, ICD-10-CM, and HCPCS code tells a story—about patient conditions, provider decision-making, and the value of care delivered.
As payers continue to focus on:
-
- Accuracy
- Medical necessity
- Documentation integrity
- Value-based care alignment
…the margin for coding errors is shrinking.
By 2026, practices that fail to align with updated coding guidelines risk:
-
- Increased claim denials
- Underpayments
- Compliance audits
- Revenue leakage
- Provider burnout due to rework
Understanding upcoming changes now allows practices to prepare proactively rather than react defensively later.
1. Continued Expansion and Refinement of ICD-10-CM Codes
ICD-10-CM updates remain one of the most significant annual changes in medical coding, and the trend continues into 2026.
What’s Changing
-
- New diagnosis codes for emerging conditions
- Greater specificity for existing disease categories
- Expanded social determinants of health (SDOH) coding
- Refined injury, complication, and severity classifications
These changes reflect the healthcare industry’s push toward more detailed patient data and population health insights.
Why It Matters
Using outdated or nonspecific ICD-10 codes can result in:
-
- Claim rejections
- Down coding
- Missed risk adjustment opportunities
- Incomplete patient records
What Practices Should Do Now
-
- Review annual ICD-10 updates thoroughly
- Educate providers on documentation specificity
- Ensure EHR systems are updated and mapped correctly
- Train coders on new code selection rules
2. Evaluation and Management (E/M) Coding: Ongoing Clarifications
Although major E/M changes were introduced earlier, clarifications and refinements continue to impact coding accuracy as we approach 2026.
Key Focus Areas
-
- Medical Decision Making (MDM) interpretation
- Time-based documentation requirements
- Split/shared visit reporting
- Modifier usage clarity
Auditors are paying closer attention to whether documentation truly supports the selected E/M level.
Common Risk Areas
-
- Over-reliance on time without adequate support
- Misinterpreting “moderate” vs. “high” MDM
- Inconsistent documentation between providers
Best Practices
-
- Align documentation templates with updated E/M guidelines
- Conduct internal E/M audits regularly
- Train providers on real-world examples, not just theory
- Encourage clarity over volume in clinical notes
3. Telehealth and Virtual Care Coding Evolution
Telehealth is no longer considered a temporary solution—it’s now a permanent part of care delivery. However, coding and reimbursement expectations continue to evolve.
What’s Changing
-
- Refinement of telehealth CPT codes
- Clearer rules around audio-only services
- Location and place-of-service reporting updates
- Documentation standards for virtual encounters
Why This Update Is Critical
Incorrect telehealth coding can lead to:
-
- Denied claims
- Reduced reimbursement
- Compliance risks during payer audits
What Practices Must Review
-
- Payer-specific telehealth policies
- Appropriate modifiers and POS codes
- Documentation requirements unique to virtual visits
- Eligibility criteria for remote services
Preparing now ensures telehealth revenue remains stable and compliant through 2026.
4. Increased Emphasis on Social Determinants of Health (SDOH) Coding
Healthcare is shifting toward whole-person care, and coding is following that direction.
What’s New
-
- Expanded Z-codes related to housing, food insecurity, employment, and social support
- Increased payer interest in capturing SDOH data
- Integration of SDOH coding into risk-based reimbursement models
Why This Matters
SDOH codes:
-
- Improve care coordination
- Support value-based care reporting
- Enhance population health data
- Contribute to risk adjustment accuracy
Action Steps for Practices
-
- Train providers to document SDOH factors clearly
- Encourage appropriate use of Z-codes
- Coordinate with care management teams
- Update intake forms to capture relevant data
5. Risk Adjustment Coding Scrutiny Is Increasing
Risk adjustment coding is under intense review as payers and regulators focus on accuracy and integrity.
What’s Changing
-
- Tighter documentation requirements
- Increased audits related to Hierarchical Condition Categories (HCCs)
- Greater emphasis on annual condition recapture
Common Challenges
-
- Unsupported diagnoses
- Copy-forward documentation errors
- Missing treatment plans
- Inconsistent problem list maintenance
Best Practices Before 2026
-
- Conduct regular risk adjustment audits
- Educate providers on “MEAT” documentation principles
- Ensure chronic conditions are assessed annually
- Clean up problem lists to reflect current conditions
6. Modifier Usage Updates and Increased Monitoring
Modifiers play a critical role in accurate reimbursement, but misuse is a common audit trigger.
Modifiers Under Scrutiny
-
- Modifier 25
- Modifier 59
- X-modifiers
- Modifier 26 and TC
Why This Is Important
Incorrect modifier usage can:
-
- Trigger payer audits
- Result in claim denials or recoupments
- Delay reimbursement
What Practices Should Do
-
- Review modifier guidelines regularly
- Provide targeted modifier training
- Perform claim-level audits
- Avoid “default” modifier usage without documentation support
7. Surgical and Procedural Coding Refinements
Procedural coding continues to evolve with advances in medical technology and surgical techniques.
Key Trends
-
- New CPT codes for minimally invasive procedures
- Bundling and unbundling rule updates
- Clarifications around global surgical packages
Risk Areas
-
- Unbundling procedures incorrectly
- Misunderstanding global period rules
- Failing to report add-on codes properly
Preparation Tips
-
- Stay updated on CPT changes annually
- Cross-check National Correct Coding Initiative (NCCI) edits
- Train surgical teams and coders together
- Review operative notes for clarity and completeness
8. Documentation Standards Are Becoming More Stringent
As coding rules evolve, documentation expectations are rising to match them.
What’s Driving This Change
-
- Increased payer audits
- Value-based care reporting
- Legal and compliance requirements
Key Documentation Focus Areas
-
- Medical necessity
- Clinical rationale
- Treatment plans
- Outcomes and follow-up
What Practices Can Do
-
- Standardize documentation templates
- Provide provider feedback regularly
- Encourage concise yet complete notes
- Avoid copy-paste errors
9. Coding Compliance and Audit Readiness
Compliance is no longer just about avoiding penalties—it’s about building sustainable revenue systems.
What’s New
-
- More frequent payer audits
- Advanced data analytics used by payers
- Higher penalties for repeated errors
Audit-Ready Practices
-
- Perform internal coding audits quarterly
- Maintain updated compliance policies
- Document corrective actions
- Offer continuous coder education
Being proactive significantly reduces audit risk.
10. Technology and Coding Workflow Integration
Technology is playing a larger role in coding accuracy—but it must be used correctly.
Trends to Watch
-
- Computer-Assisted Coding (CAC) tools
- EHR-integrated coding alerts
- Automated claim scrubbing
- Data-driven denial prevention
Important Reminder
Technology supports coders—it does not replace them.
Best Approach
-
- Combine automation with human oversight
- Validate system-generated codes
- Monitor performance metrics regularly
- Update workflows based on real-world results
How Practices Should Prepare Before 2026
Preparation is not about reacting to change—it’s about planning for it.
Key Action Steps
-
- Review all annual coding updates
- Invest in ongoing coder and provider education
- Conduct regular audits
- Update policies and workflows
- Encourage collaboration between clinical and billing teams
Practices that take these steps now will enter 2026 with confidence, compliance, and financial stability.
Medical coding is evolving rapidly, and the changes ahead of 2026 are shaping the future of healthcare reimbursement. Staying informed is no longer enough—practices must actively adapt.
By reviewing these top medical coding updates now, healthcare organizations can:
-
- Reduce denials
- Improve documentation accuracy
- Strengthen compliance
- Optimize revenue
- Support better patient care
The practices that succeed in 2026 will be the ones that treat medical coding not as a back-office task—but as a strategic pillar of healthcare operations.