In 2026, claim denials are no longer viewed as an unavoidable part of healthcare operations—they are increasingly seen as a preventable revenue leak. As margins tighten, payer scrutiny intensifies, and patient expectations rise, healthcare organizations are under more pressure than ever to get billing right the first time.
Yet, despite advancements in technology and data availability, claim denial rates remain stubbornly high across the industry. According to internal payer trend analyses and RCM benchmarks, denial rates continue to hover between 8% and 15%, with a significant portion classified as avoidable. Each denied claim represents more than delayed revenue—it means additional labor, increased costs, frustrated staff, and often a negative patient experience.
The good news? In 2026, reducing claim denials is no longer just about fixing errors after the fact. It’s about smarter medical billing strategies that combine people, process, data, and technology into a proactive, denial-resistant revenue cycle.
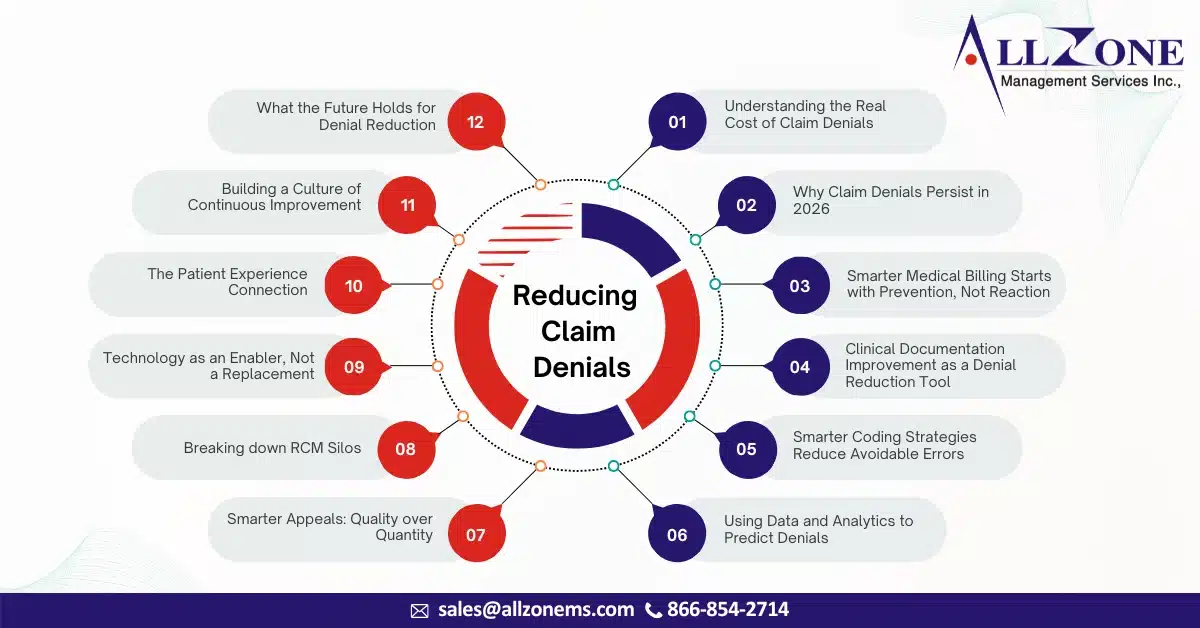
This newsletter explores how healthcare organizations can significantly reduce claim denials in 2026 by adopting smarter, more strategic medical billing practices—without losing the human touch that remains critical to success.
Understanding the Real Cost of Claim Denials
Before addressing solutions, it’s essential to understand why claim denials are such a critical issue in today’s healthcare environment.
A denied claim doesn’t just delay payment—it can cost three to five times more to rework than a clean claim. Multiply that across thousands of claims each month, and the financial impact becomes staggering. Even worse, many denied claims are never appealed or recovered, resulting in permanent revenue loss.
Beyond finances, denials also affect:
-
- Staff morale, as billing teams spend hours reworking preventable errors
- Provider productivity, due to repeated documentation requests
- Patient satisfaction, when balances are shifted to them unfairly
- Compliance risk, especially when denial trends go unnoticed
In 2026, smarter organizations recognize that denial reduction isn’t a back-end cleanup task—it’s a front-end strategy embedded throughout the entire revenue cycle.
Why Claim Denials Persist in 2026
Despite years of awareness, claim denials remain common because healthcare billing is becoming more complex, not less. Several factors continue to drive denial rates upward:
1. Constantly Changing Payer Rules
Payers update coverage policies, prior authorization requirements, and medical necessity guidelines frequently. Without real-time visibility and education, billing teams struggle to keep up.
2. Incomplete or Inaccurate Documentation
Even highly skilled clinicians may unintentionally omit key details required to support coding and medical necessity.
3: Eligibility and Authorization Gaps
Small mistakes in insurance verification or missed authorizations can result in automatic denials.
4. Coding Errors and Mismatches
ICD-10, CPT, and modifier usage continue to evolve. Incorrect combinations or outdated codes are still a leading cause of denials.
5. Siloed RCM Processes
When front-end, mid-cycle, and back-end teams operate independently, errors slip through unnoticed until claims are denied.
The reality in 2026 is clear: denials are rarely caused by a single mistake—they’re usually the result of disconnected processes.
Smarter Medical Billing Starts with Prevention, Not Reaction
The most successful healthcare organizations in 2026 have shifted their mindset from denial management to denial prevention. Instead of focusing solely on appeals, they invest in strategies that reduce the likelihood of denials occurring at all.
- Strengthening Front-End Accuracy
Denial prevention begins before the patient even walks through the door.
Smarter billing teams prioritize:
-
- Real-time eligibility verification
- Accurate demographic and insurance data capture
- Proactive identification of authorization requirements
- Clear financial communication with patients
Front-end accuracy is no longer a clerical function—it’s a strategic revenue protection role. In 2026, organizations that invest in training and accountability at registration see dramatic reductions in downstream denials.
Clinical Documentation Improvement as a Denial Reduction Tool
One of the most overlooked strategies for reducing claim denials is clinical documentation improvement (CDI).
In 2026, payers are more focused than ever on:
-
- Medical necessity
- Risk adjustment accuracy
- Severity of illness and complexity
When documentation fails to tell the full clinical story, claims are denied—even if the care provided was entirely appropriate.
Smarter organizations bridge the gap between providers and billing teams by:
-
- Implementing physician-friendly documentation guidelines
- Using concurrent documentation reviews
- Educating providers on payer-specific expectations
- Offering feedback loops instead of punitive audits
The goal is not to burden clinicians, but to support them in telling a complete and defensible patient story.
Smarter Coding Strategies Reduce Avoidable Errors
In 2026, coding accuracy is about far more than code selection—it’s about context, compliance, and consistency.
Leading billing teams adopt smarter coding strategies such as:
-
- Routine internal coding audits focused on denial trends
- Specialty-specific coding education
- Standardized modifier usage policies
- Alignment between coding and payer contract terms
Rather than treating coding as an isolated function, smart organizations integrate coders into denial analysis discussions. When coders understand which codes are most frequently denied—and why—they become proactive partners in prevention.
Using Data and Analytics to Predict Denials
One of the biggest shifts in 2026 is the use of denial analytics not just to report problems, but to predict them.
Smarter medical billing teams track:
-
- Denials by payer, provider, procedure, and location
- Root causes instead of surface-level reasons
- First-pass claim acceptance rates
- Trends over time rather than isolated incidents
By analyzing patterns, organizations can identify:
-
- High-risk claims before submission
- Payers with inconsistent denial behavior
- Training gaps among staff or providers
This data-driven approach transforms denial management from a reactive task into a strategic advantage.
Smarter Appeals: Quality over Quantity
Even with the best prevention strategies, some denials are inevitable. In 2026, smarter organizations focus on high-impact appeals, not volume-based rework.
Effective appeal strategies include:
-
- Prioritizing denials with the highest recovery potential
- Using payer-specific appeal templates
- Attaching strong clinical documentation upfront
- Tracking appeal success rates by denial type
Rather than appealing everything, successful billing teams ask a smarter question:
“Which denials are worth fighting—and how can we prevent them next time?”
Breaking down RCM Silos
One of the most powerful denial reduction strategies in 2026 is cross-functional collaboration.
Smarter organizations bring together:
-
- Front-end staff
- Coders
- Billers
- Clinical teams
- Compliance and quality leaders
Regular denial review meetings foster shared accountability and faster problem resolution. When everyone understands how their role affects claim outcomes, denials drop naturally.
In this collaborative model, denials are no longer “billing’s problem”—they’re a system-wide responsibility.
Technology as an Enabler, Not a Replacement
Technology plays a vital role in smarter medical billing in 2026, but successful organizations understand that tools alone don’t solve problems.
The most effective teams use technology to:
-
- Flag missing documentation before claim submission
- Validate coding and modifier combinations
- Monitor payer policy updates
- Automate routine checks while preserving human oversight
Technology supports staff—it doesn’t replace critical thinking. The human review remains essential for complex cases, nuanced payer rules, and patient-specific considerations.
The Patient Experience Connection
Reducing claim denials isn’t just about revenue—it’s also about patients.
Denied claims often result in:
-
- Unexpected patient balances
- Confusing statements
- Delayed financial resolution
Smarter billing strategies improve transparency and trust by:
-
- Ensuring claims are accurate the first time
- Reducing re-billing cycles
- Communicating clearly with patients about coverage and responsibility
In 2026, patient satisfaction and revenue integrity are deeply connected.
Building a Culture of Continuous Improvement
The most successful denial reduction programs are not one-time initiatives—they’re ongoing commitments.
Smarter organizations in 2026 foster a culture that:
-
- Encourages learning from denials instead of assigning blame
- Invests in continuous education
- Celebrates improvements in clean claim rates
- Adapts quickly to payer and regulatory changes
Denials become data points—not failures.
What the Future Holds for Denial Reduction
As healthcare continues to evolve, denial prevention will become even more critical. Payers will demand greater accuracy, regulators will expect stronger compliance, and patients will insist on transparency.
Organizations that embrace smarter medical billing strategies today will:
-
- Improve cash flow
- Reduce administrative burden
- Strengthen compliance
- Enhance patient trust
In 2026, reducing claim denials is no longer about working harder—it’s about working smarter.
Claim denials are not an unavoidable cost of doing business in healthcare. They are signals—pointing to gaps in process, communication, or strategy.
By focusing on smarter medical billing practices—prevention-first workflows, data-driven insights, collaborative teams, and thoughtful use of technology—healthcare organizations can dramatically reduce denials while improving efficiency and patient satisfaction.
The path forward isn’t perfect, but it’s clear.
And in 2026, smarter billing isn’t optional—it’s essential.