J-codes are a critical part of medical billing, representing a specific set of alphanumeric codes used to bill for drugs and non-orally administered medications. Understanding them is crucial for accurate claims submission and proper reimbursement in healthcare. This blog post will dive into what J-codes are, how they work, their importance, and key considerations for […]
An AI medical scribe for clinical documentation is helping a healthcare system prevent claim denials while giving clinicians more face-to-face time with their patients. The healthcare system, based in Yuma County, Arizona, is a nonprofit with nearly 500 providers, 430 inpatient beds, and 45 outpatient clinics. Its goal is to reduce clinician burnout, which is […]
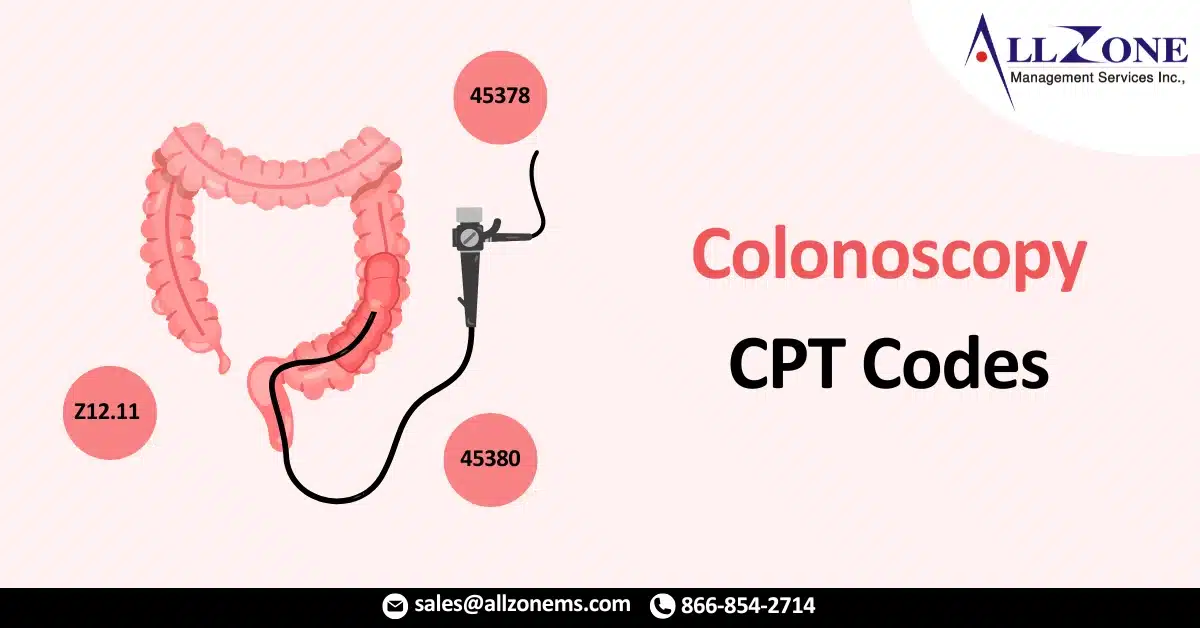
In the world of medical billing and coding, proper documentation and coding of procedures is essential for timely reimbursements and compliance. One such critical procedure is the colonoscopy, a diagnostic and preventive test widely used in the detection of colorectal conditions such as cancer, polyps, inflammatory bowel disease, and more. To ensure accurate reimbursement and […]
Migraines are one of the most common neurological conditions affecting millions of individuals worldwide. For healthcare providers and medical coders, accurately documenting and assigning migraine ICD 10 codes is essential for proper treatment and reimbursement. At Allzone, we specialize in providing expert medical billing and coding services that help streamline processes and maximize revenue. In […]
In the intricate world of medical billing and coding, understanding specific CPT (Current Procedural Terminology) codes is paramount for healthcare providers and patients alike. Among these, CPT code 90791 holds a significant place, representing a crucial initial step in mental health care: the psychiatric diagnostic evaluation. This comprehensive guide will delve into the nuances of […]
In essence, the insurance company you billed believes another insurer is primarily responsible for the payment. Understanding and effectively managing CO 22 denial code is critical for maintaining a healthy revenue cycle and ensuring timely reimbursements. This comprehensive guide will break down the CO 22 denial code, explore its common causes, and provide actionable strategies […]
In today’s dynamic healthcare environment, managing accounts receivable (AR) is more than just a financial function—it’s a critical component of sustaining a profitable and compliant medical practice. Delays in reimbursements, claim denials, and inefficient billing processes can drain resources and hinder growth. That’s where AR recovery in medical billing plays a vital role. At Allzone […]
In the complex world of medical billing, accurate documentation is essential for timely reimbursements and claim acceptance. One of the most critical tools in hospital and institutional billing is the UB-04 claim form, also known as the CMS-1450. Whether you’re a healthcare provider, billing professional, or medical coder, understanding this form is crucial for ensuring […]
Coronary Artery Disease (CAD) is one of the most common and serious forms of heart disease. In the medical billing and coding world, accurately documenting and coding CAD is critical for correct reimbursement, tracking patient outcomes, and ensuring compliance with healthcare regulations. The ICD-10 code for CAD serves as a fundamental identifier for healthcare providers […]
Mammography, a vital screening tool in the early detection of breast cancer, is typically billed using CPT codes and HCPCS Level II (G codes). However, the correct use of G codes for mammograms—particularly for Medicare beneficiaries—is often a source of confusion for healthcare providers and billing teams. In this comprehensive guide, we’ll explore: The difference […]