Accounts Receivable (AR) days directly impact cash flow and overall financial health. The longer a claim sits in AR, the more challenging it becomes to collect revenue, leading to cash flow disruptions, operational inefficiencies, and reduced profitability. Therefore, it’s crucial for businesses to actively work to reduce AR days and improve their financial performance. With […]
As the healthcare landscape continues to evolve at an unprecedented pace, 2025 is poised to be a landmark year for revenue cycle management (RCM). With regulatory changes, emerging technologies, and shifting patient expectations, healthcare providers and RCM professionals must stay ahead of the curve to optimize financial performance and patient care. In this newsletter, we […]
A well-managed A/R process ensures timely cash flow, reduces administrative burdens, and maintains the stability of a healthcare practice. However, many healthcare practices still struggle with outdated, manual A/R management processes that can lead to inefficiencies, errors, and delayed payments. In recent years, Revenue Cycle Management (RCM) automation has emerged as a game-changer in addressing […]
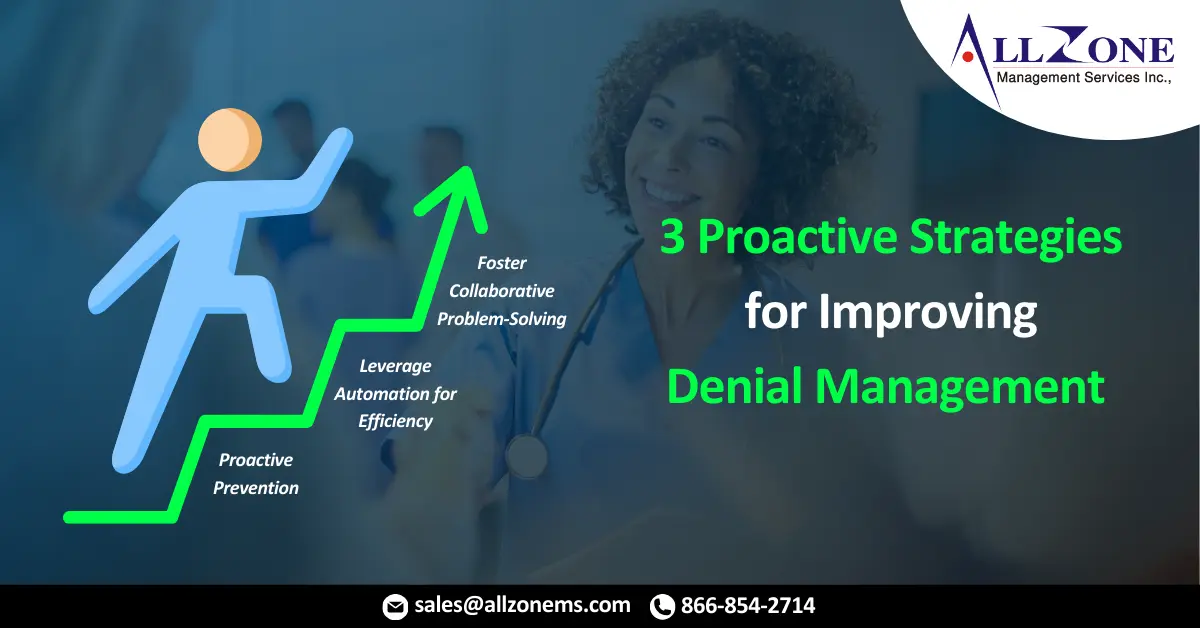
In the ever-evolving field of medical billing, denied claims remain a significant obstacle for healthcare providers. Studies reveal that over 10% of claims face initial rejection by insurers, leading to revenue losses, administrative strain, and frustration for all stakeholders. To mitigate these challenges and ensure financial stability, an effective denial management process is essential. However, […]
However, AI in Revenue Cycle Management is emerging as a transformative solution. By automating repetitive tasks, improving accuracy, and providing actionable insights, AI is helping healthcare organizations streamline their processes and tackle these challenges more effectively. Revenue Cycle Management (RCM) is a cornerstone of healthcare operations, yet the growing complexity of today’s healthcare landscape poses […]
2025 promises to bring transformative changes to Revenue Cycle Management (RCM) in an ever-evolving healthcare landscape. To navigate financial complexities and enhance patient satisfaction, healthcare providers must stay on top of emerging 2025 Revenue Cycle Management trends as they emphasize efficiency, transparency, and patient-centered care. In this newsletter, we explore key RCM trends that will […]
Medical coding denials are a common challenge for healthcare providers and revenue cycle management (RCM) teams. They can disrupt cash flow, delay reimbursements, and increase administrative workloads. Avoiding these denials requires a proactive approach that addresses their root causes, ensures compliance with regulations, and fosters a culture of continuous improvement. In this blog, we’ll explore […]
End to end RCM (Revenue Cycle Management) encompasses every step in the healthcare payment process, from patient registration to final reimbursement. By adopting a comprehensive RCM approach, healthcare organizations can improve cash flow, minimize errors, and ensure compliance with ever-changing regulations. This blog will explore the components, benefits, and best practices for implementing an end […]
Technology advancements, evolving healthcare policies, and the ongoing shift to value-based care have all contributed to rapid changes in Revenue Cycle Management (RCM). In 2025 and beyond, healthcare companies will face both unprecedented challenges and opportunities for innovation and streamlined RCM processes. Organizations like Allzone Management Services, with its robust Allzone’s RCM Solutions, must stay […]
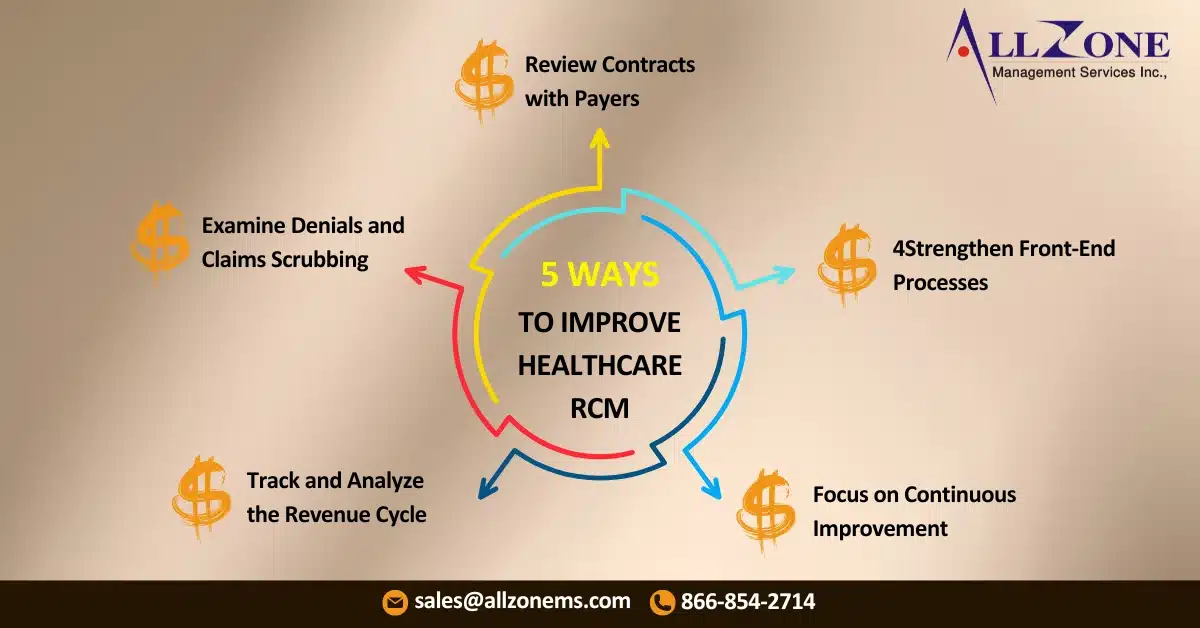
The healthcare industry operates under a unique framework. Unlike traditional businesses where customers pay directly for a product or service, healthcare providers navigate a complex system involving multiple players, including payers, claims management, and reimbursements. To Improve Revenue Cycle Management, healthcare providers must understand this intricate system and implement efficient strategies to optimize their revenue […]