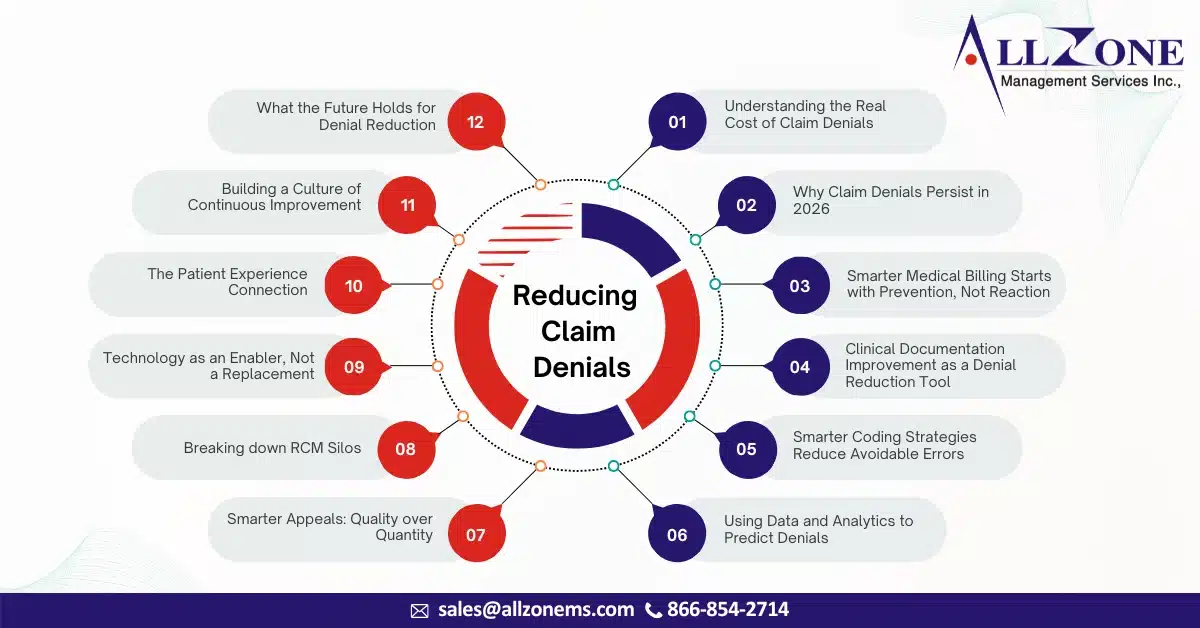
In 2026, claim denials are no longer viewed as an unavoidable part of healthcare operations—they are increasingly seen as a preventable revenue leak. As margins tighten, payer scrutiny intensifies, and patient expectations rise, healthcare organizations are under more pressure than ever to get billing right the first time. Yet, despite advancements in technology and data […]
Medical claim denials continue to pose a serious challenge for healthcare providers striving to maintain steady cash flow and financial stability. As payer policies become increasingly complex, documentation standards tighten, and reimbursement models evolve, even a minor oversight in billing or coding can result in delayed payments or lost revenue. Effective denial management in medical […]
As the year comes to a close, healthcare organizations feel the same pressure they always do: closing out accounts, speeding up collections, settling outstanding claims, and getting rid of operational bottlenecks before January 1st. The last three months of the year are often the most important for a company’s financial health. What happens now will […]
Accurate modifier usage is one of the most important elements in achieving clean claim submissions and full reimbursement in surgical billing. Among the lesser-used but extremely important surgical modifiers is Modifier 81 – Minimum Assistant Surgeon. Many practices overlook or misuse this modifier, leading to preventable denials, delayed payments, and compliance issues. This comprehensive guide […]
Introduction In medical billing, modifiers play a vital role in explaining the circumstances under which a service or procedure was performed. One such important modifier is Modifier 76, which helps billers and coders indicate when a repeat procedure or service is performed by the same physician or qualified healthcare professional. Accurate use of Modifier 76 […]
In the complex world of medical billing, claim denials are one of the biggest challenges healthcare providers face. Among them, CO-97 denial code is one of the most frequent and confusing denials providers encounter. A denied claim not only disrupts cash flow but also leads to additional administrative costs and potential compliance risks. To minimize […]
In the healthcare revenue cycle, denials are inevitable — but how you manage them makes all the difference. A common discussion in this space centers around Denial Prevention vs. Denial Facilitation, two strategies that, while they may sound similar, have distinct purposes and outcomes. Understanding and effectively applying both can drastically improve your practice’s cash […]
Navigating the complexities of denials management can feel overwhelming for revenue cycle leaders seeking effective solutions. Instead of chasing quick fixes, a structured, methodical approach is essential for building a sustainable and impactful denials management strategy. Implementing a Robust Denials Management Solution is key to achieving this, as it provides the necessary framework for a […]
Claim denials pose a substantial threat to the financial health of medical practices. Effective medical claim denial management is crucial for protecting revenue, streamlining operations, and maintaining positive payer relationships. This comprehensive guide outlines a strategic approach to reducing denials, managing appeals, and safeguarding your practice’s financial stability, with a strong focus on effective medical […]
The healthcare industry is on the brink of a technological transformation, with artificial intelligence (AI) driving unprecedented efficiency and accuracy in medical coding. As we enter 2025, AI-powered automation is no longer just a trend—it is becoming the backbone of modern medical coding operations. From accelerating coding workflows and minimizing human error to ensuring compliance […]