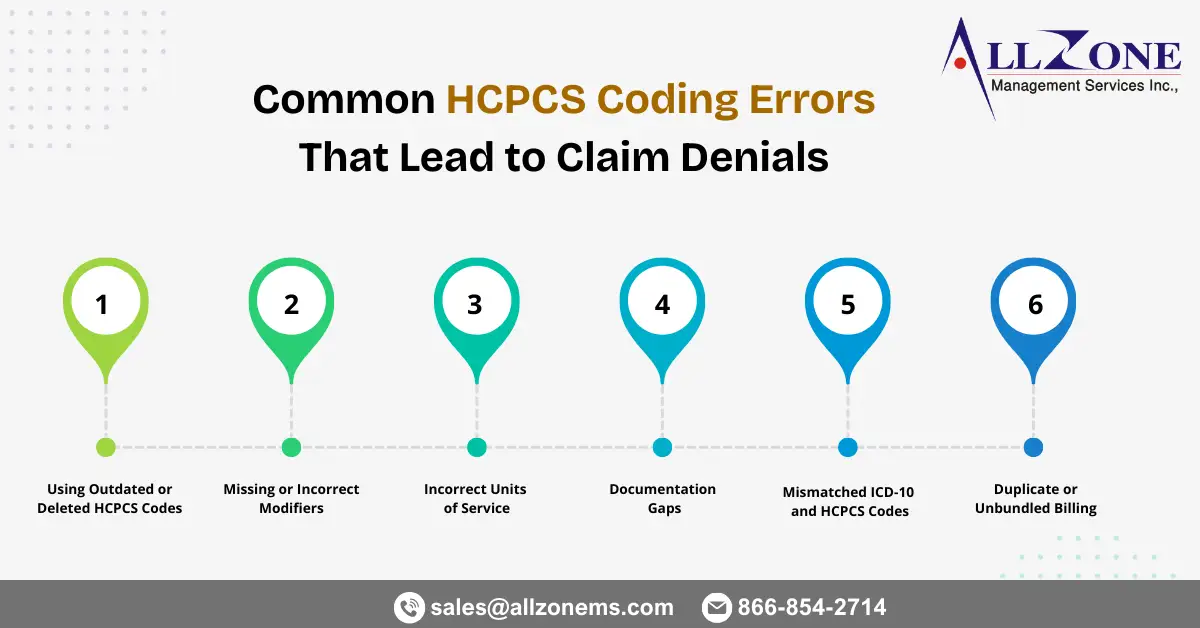
Healthcare organizations rely heavily on accurate coding to ensure timely reimbursement. While CPT and ICD-10 codes often receive most of the attention, HCPCS Level II codes play an equally critical role in billing for supplies, medications, durable medical equipment (DME), ambulance services, and other non-physician services. Even small HCPCS mistakes can trigger claim rejections, payment […]
Here’s your rephrased, expanded, and more natural (human-written style) version with smoother flow, stronger transitions, and added depth. I kept your structure but enriched the narrative, added examples, and improved readability while keeping it newsletter/blog-friendly. In 2026, healthcare organizations are dealing with a challenge that feels familiar—but far more intense than before. Claims are becoming […]
In today’s complex healthcare billing environment, patients are increasingly paying out-of-pocket for medical services and later seeking reimbursement from their insurance plans. This shift has made the Direct Member Reimbursement (DMR) form an essential component of the revenue cycle for both patients and healthcare providers. A Direct Member Reimbursement form allows insured members to request […]
Enteral and parenteral therapies play a critical role in the treatment of patients who cannot meet their nutritional or medication needs through normal oral intake. From patients with gastrointestinal disorders to those requiring long-term intravenous nutrition, these therapies are essential for sustaining life and improving clinical outcomes. However, billing for these services can be complex, […]
Accurate modifier usage is one of the most important elements in achieving clean claim submissions and full reimbursement in surgical billing. Among the lesser-used but extremely important surgical modifiers is Modifier 81 – Minimum Assistant Surgeon. Many practices overlook or misuse this modifier, leading to preventable denials, delayed payments, and compliance issues. This comprehensive guide […]
Introduction In the complex world of healthcare reimbursement, coding accuracy is critical to ensure proper payment and compliance. Among the various code sets used, HCPCS K Codes hold a special place for their role in billing durable medical equipment (DME) and other specific supplies. These codes are often overlooked but play an essential part in […]
In the complex world of healthcare, accuracy in medical coding is not just about compliance—it’s the foundation of timely reimbursements and a healthy revenue cycle. Among the most common patient complaints is hip pain, which often leads to diagnostic evaluations and treatment claims. Properly using the ICD-10 code for right hip pain (M25.551) is crucial […]
Total knee arthroplasty (TKA), also known as total knee replacement, is one of the most commonly performed orthopedic procedures in the United States. With the rising number of patients suffering from osteoarthritis, rheumatoid arthritis, and other degenerative joint diseases, the demand for accurate coding and billing for knee replacement surgeries has never been greater. For […]
Introduction In medical billing, claim rejections and denials are inevitable—but understanding why they occur is the key to fixing them. One of the most important tools for decoding these denials is the Claim Adjustment Reason Code (CARC). Each CARC provides specific information about why a claim or a service line was adjusted, denied, or paid […]
In the complex world of medical billing, claim denials are one of the biggest challenges healthcare providers face. Among them, CO-97 denial code is one of the most frequent and confusing denials providers encounter. A denied claim not only disrupts cash flow but also leads to additional administrative costs and potential compliance risks. To minimize […]