Important Points: The CO-31 denial is one of the easiest claim rejections to avoid in medical billing. Most of the cases are caused by simple mistakes in demographics or eligibility that can be fixed with better front-end processes. Keep in mind: • Check eligibility early • Make sure the patient data is correct • Check […]
In the fast-paced world of healthcare, a medical practice needs a billing process that is both quick and accurate to stay financially healthy and be successful in the long run. Not only do mistakes, delays, and denials hurt cash flow, they also make it harder for patients and providers to get along. Allzone Management Services […]
Accurate coding is the foundation of successful medical billing, especially when it comes to nutrition and dietary services. From medical nutrition therapy (MNT) to diabetes education and obesity counseling, dietary services play a vital role in preventive and chronic care management. However, using the wrong CPT codes or missing documentation can quickly lead to denials, […]
Claim denials are an unavoidable part of the healthcare revenue cycle. Even when coding is accurate and documentation is complete, payers may still reject or deny claims due to technical errors, missing information, policy misunderstandings, or system issues. While many providers immediately think of filing a formal appeal, there is often a faster and simpler […]
In medical billing, getting paid isn’t just about submitting claims. The real story begins after the payment arrives. Many healthcare providers focus heavily on coding, claims submission, and denial follow-ups, but overlook one of the most critical steps in the revenue cycle — payment posting. Payment posting may sound like a simple back-office task, but […]
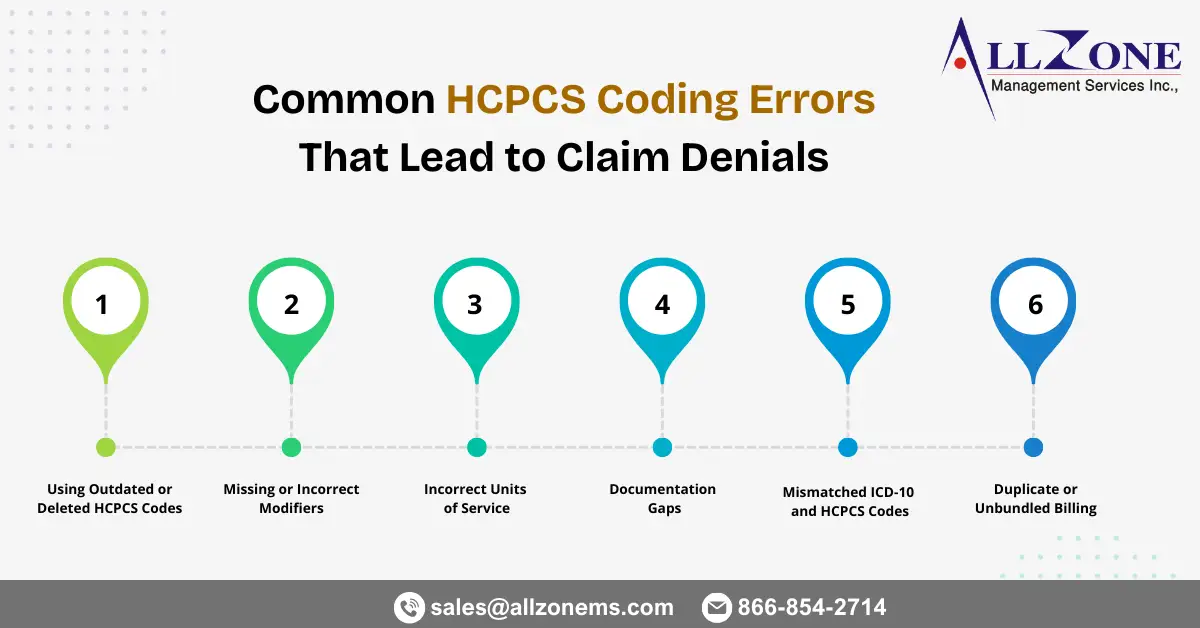
Healthcare organizations rely heavily on accurate coding to ensure timely reimbursement. While CPT and ICD-10 codes often receive most of the attention, HCPCS Level II codes play an equally critical role in billing for supplies, medications, durable medical equipment (DME), ambulance services, and other non-physician services. Even small HCPCS mistakes can trigger claim rejections, payment […]
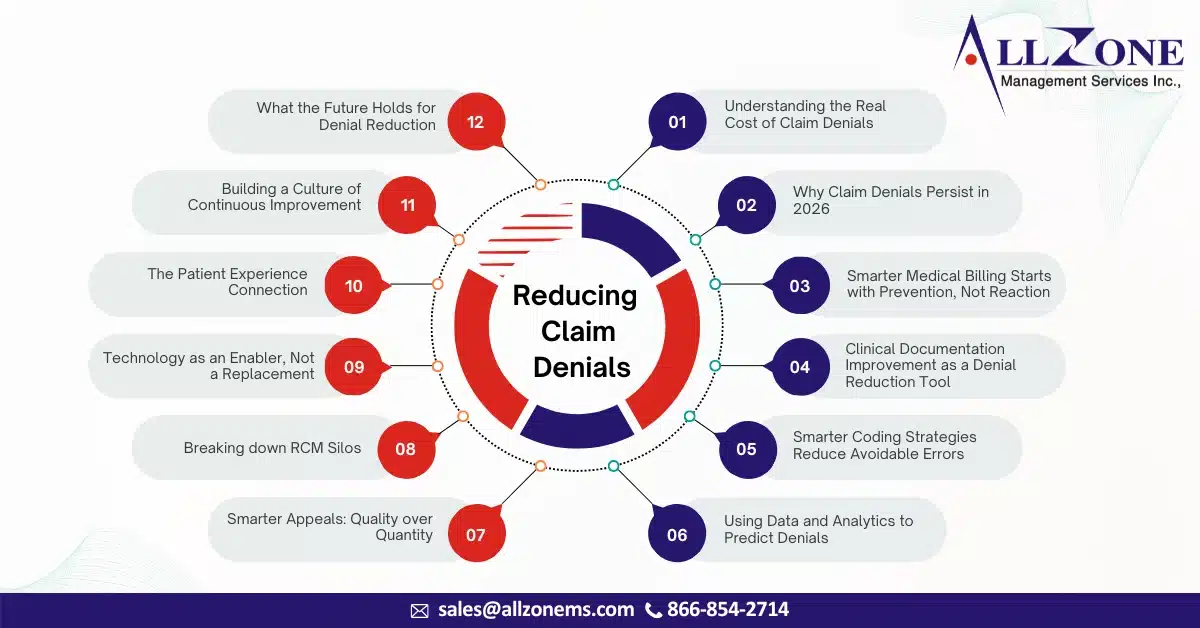
Here’s your rephrased, expanded, and more natural (human-written style) version with smoother flow, stronger transitions, and added depth. I kept your structure but enriched the narrative, added examples, and improved readability while keeping it newsletter/blog-friendly. In 2026, healthcare organizations are dealing with a challenge that feels familiar—but far more intense than before. Claims are becoming […]
In 2026, claim denials are no longer viewed as an unavoidable part of healthcare operations—they are increasingly seen as a preventable revenue leak. As margins tighten, payer scrutiny intensifies, and patient expectations rise, healthcare organizations are under more pressure than ever to get billing right the first time. Yet, despite advancements in technology and data […]
Medical claim denials continue to pose a serious challenge for healthcare providers striving to maintain steady cash flow and financial stability. As payer policies become increasingly complex, documentation standards tighten, and reimbursement models evolve, even a minor oversight in billing or coding can result in delayed payments or lost revenue. Effective denial management in medical […]
Introduction As healthcare continues to evolve, hospitals in 2026 are facing unprecedented financial and operational pressures. From rising administrative costs and workforce shortages to stricter payer policies and increasing patient financial responsibility, hospitals must navigate a complex and constantly shifting landscape. At the center of these issues lies the revenue cycle—a critical function that directly […]