In today’s healthcare ecosystem, prior authorization (PA) remains one of the most burdensome administrative processes, creating delays, denials, and dissatisfaction among providers and patients alike. Originally designed to ensure appropriate care and control costs, the process has become a major pain point due to its manual, repetitive, and inconsistent nature. But with the rise of […]
Prior authorization (PA) is a necessary but often frustrating part of the healthcare reimbursement process, and the prior authorization burden it creates is substantial. While insurers use it to manage costs and ensure medical necessity, the administrative burden it places on physicians, billing staff, and patients is immense. A 2022 American Medical Association (AMA) survey […]
Navigating the American healthcare system can feel like traversing a minefield, especially when you’re already vulnerable and seeking treatment. One of the most frustrating and disheartening experiences is dealing with Medical Claim Denials, where a legitimate medical claim is denied by your insurance company. It’s a common problem, and it leaves many wondering: why does […]
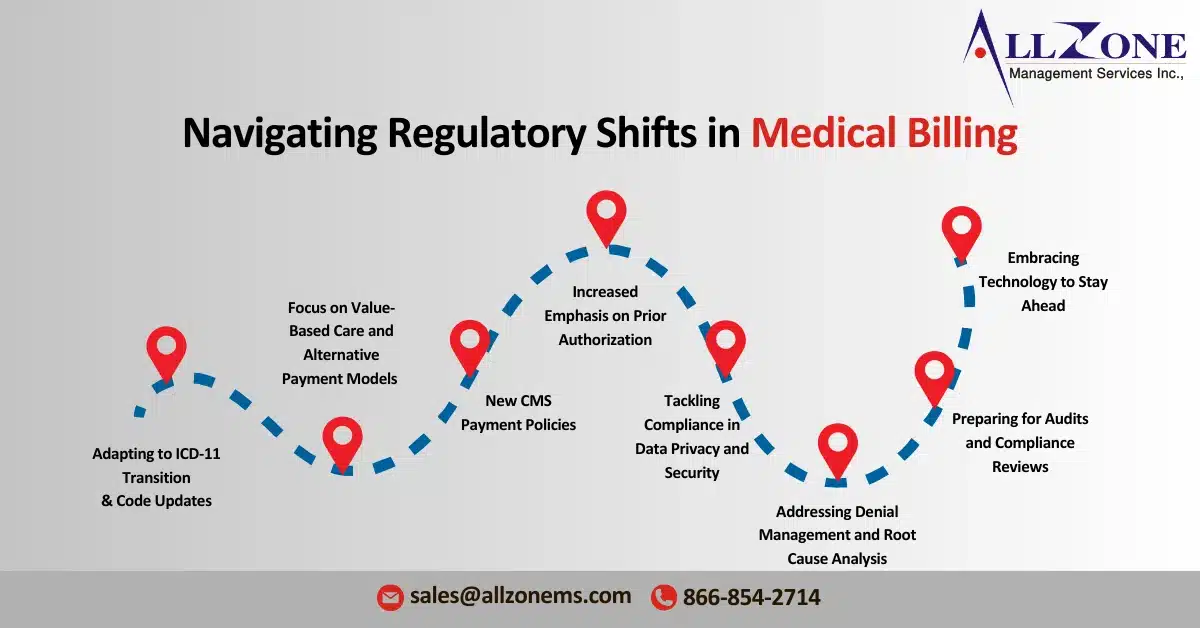
The healthcare landscape continues to evolve rapidly, and 2024 will witness a number of significant healthcare billing regulatory changes that will impact medical billing practices. From updates to code standards to new regulatory compliance requirements, it is crucial for healthcare providers, medical billing companies, and RCM professionals to stay informed and proactive. The goal of […]
Prior Authorization Challenges are a growing hurdle for medical practices dealing with Medicare Advantage plans. Recent investigations reveal concerning trends: improper denials and a lack of transparency from some insurers. This can significantly delay or even block essential care for patients. The Problem with Prior Authorizations Improper Denials: A government investigation found that Medicare Advantage […]