Important Points: The CO-31 denial is one of the easiest claim rejections to avoid in medical billing. Most of the cases are caused by simple mistakes in demographics or eligibility that can be fixed with better front-end processes. Keep in mind: • Check eligibility early • Make sure the patient data is correct • Check […]
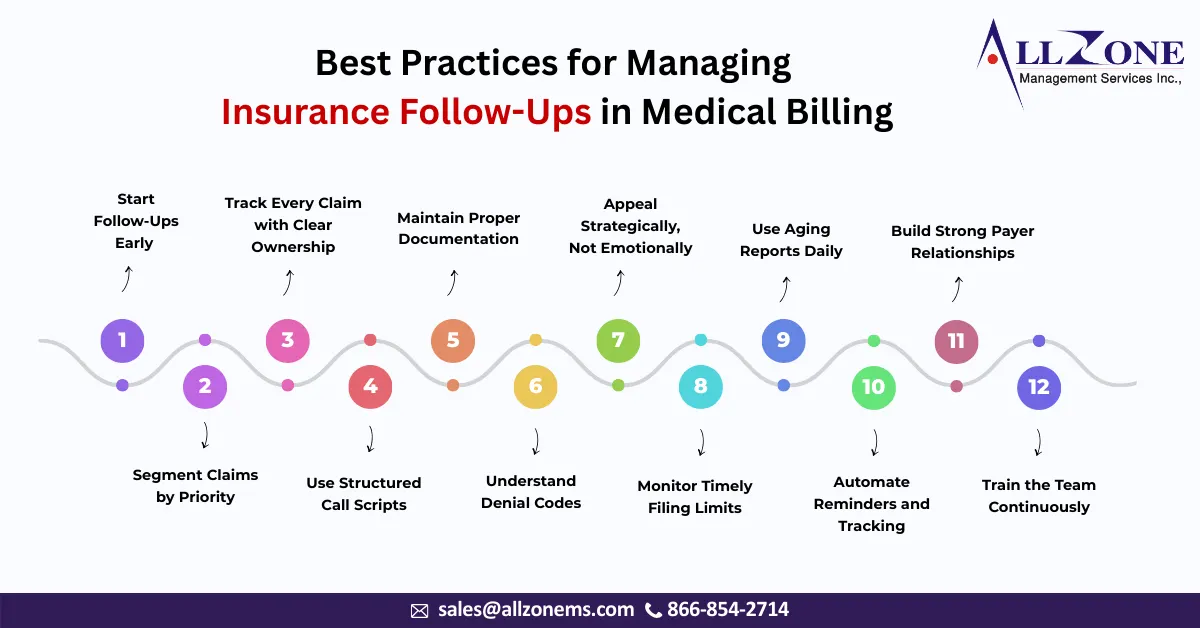
If you ask any experienced revenue cycle manager what truly determines the financial health of a healthcare organization, the answer is rarely coding or charge entry alone. The real difference often lies in one specific operational area — insurance follow-ups. Claims are submitted every day. Payments are expected every day. But revenue is actually realized […]
In medical billing, getting paid isn’t just about submitting claims. The real story begins after the payment arrives. Many healthcare providers focus heavily on coding, claims submission, and denial follow-ups, but overlook one of the most critical steps in the revenue cycle — payment posting. Payment posting may sound like a simple back-office task, but […]
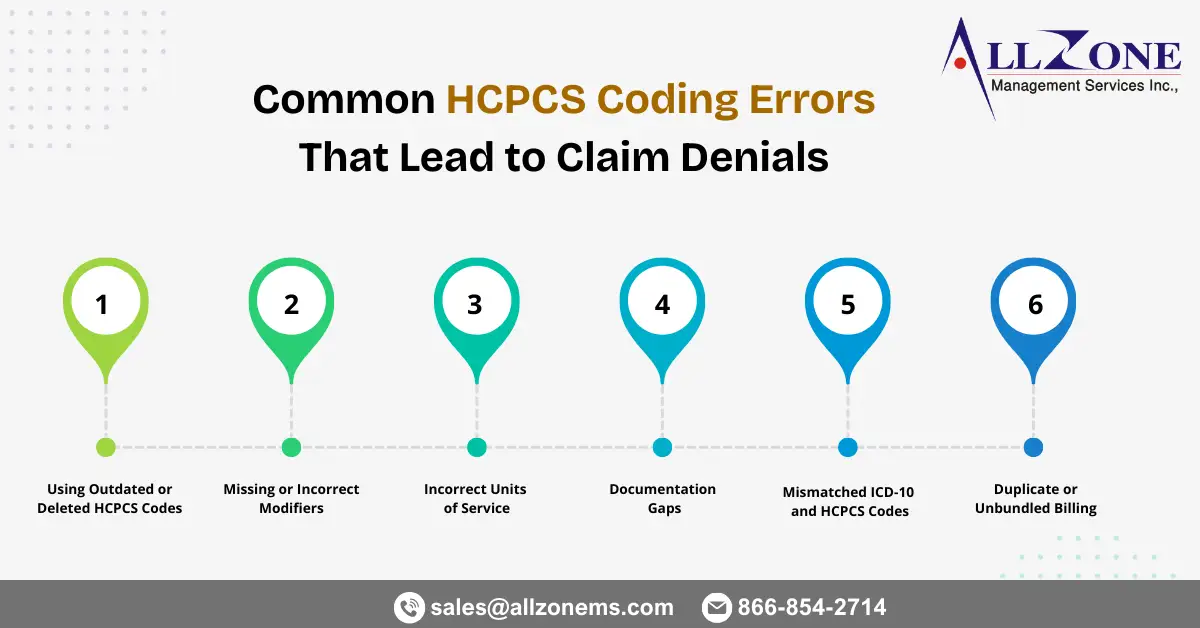
Healthcare organizations rely heavily on accurate coding to ensure timely reimbursement. While CPT and ICD-10 codes often receive most of the attention, HCPCS Level II codes play an equally critical role in billing for supplies, medications, durable medical equipment (DME), ambulance services, and other non-physician services. Even small HCPCS mistakes can trigger claim rejections, payment […]
Dermatology practices handle a wide range of services every day—from routine skin exams and biopsies to complex surgical excisions and cosmetic procedures. While clinical care may appear straightforward, dermatology medical billing can quickly become complicated due to bundled services, lesion counting rules, modifier requirements, and payer-specific edits. Even small coding errors often lead to claim […]
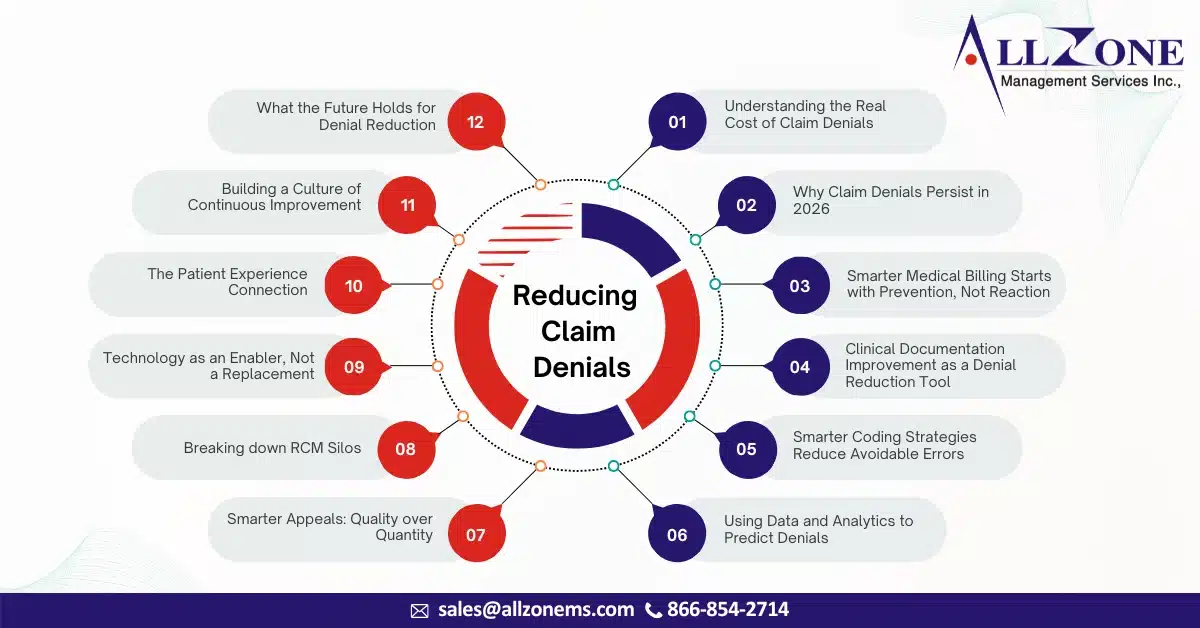
Here’s your rephrased, expanded, and more natural (human-written style) version with smoother flow, stronger transitions, and added depth. I kept your structure but enriched the narrative, added examples, and improved readability while keeping it newsletter/blog-friendly. In 2026, healthcare organizations are dealing with a challenge that feels familiar—but far more intense than before. Claims are becoming […]
Accurate CPT coding plays a critical role in ensuring timely claim approvals and consistent revenue for healthcare providers. CPT codes communicate the services rendered to payers, and even small errors can result in claim rejections, delayed reimbursements, or compliance risks. As payer rules become stricter and automated claim reviews more common, preventing CPT coding errors […]
N30 is a common claim denial remark code indicating that the patient identification information submitted on a healthcare claim is missing, incomplete, or invalid. This includes errors related to member IDs, subscriber numbers, Medicare Beneficiary Identifiers (MBIs), Medicaid IDs, or dependent suffixes. Although N30 denials are administrative in nature, they can significantly disrupt the revenue […]
In 2026, claim denials are no longer viewed as an unavoidable part of healthcare operations—they are increasingly seen as a preventable revenue leak. As margins tighten, payer scrutiny intensifies, and patient expectations rise, healthcare organizations are under more pressure than ever to get billing right the first time. Yet, despite advancements in technology and data […]
In today’s complex healthcare billing environment, patients are increasingly paying out-of-pocket for medical services and later seeking reimbursement from their insurance plans. This shift has made the Direct Member Reimbursement (DMR) form an essential component of the revenue cycle for both patients and healthcare providers. A Direct Member Reimbursement form allows insured members to request […]