How do you resolve a repeated and shooting up problem like claims denials? It’s been a fresher subject for revenue cycle management professionals for years that are only experiencing hotter with the growing pressures of staffing shortages, troubles with staff movement and instructing and developing policies and protocols at the government and payer levels. On […]
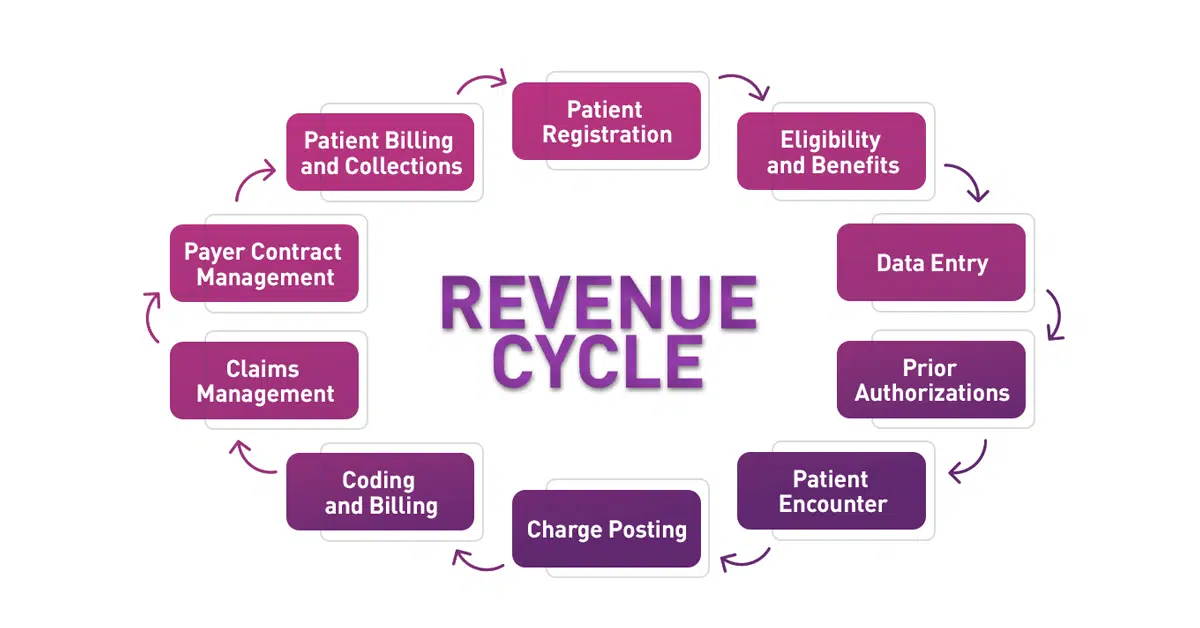
With the arise of indirect health practices such as telehealth, it is becoming increasingly indispensable to play with bill payments and claims orderly. The medical billing cycle is a complex system encompassing procedures such as medical recordkeeping and patient data processing. Medical claim processing is the keystone for healthcare insurance companies since it needs data […]
Denial rates serve as a barometer for the financial well-being of healthcare organizations. An increase in denials can have wide-ranging negative implications for an organization — impacting everything from accounts receivable to the patient experience. By preventing denials upfront, providers can realize revenue faster, boost staff efficiency and satisfaction, and reduce patient anxiety related to […]
Error-free medical billing and coding are critical characteristics of a revamped revenue cycle system. Appropriate billing and coding are not only needed in terms of compliance but are also pivotal in bringing down medical claim denials and rejections. When you take a more dynamic approach to your billing and coding operation, you not only get […]
Medical claims denials are on the rise and continue to be a costly problem for health systems. Unfortunately, the vast majority of providers focus their resources on reactive responses, working to appeal denials and recover payments after denials have already occurred. In a Becker’s Healthcare podcast an expert, discussed the problem of rising denials, why […]
While these activities oftentimes become challenging, they should help in facilitating reimbursement. This month, we’ll dive into the next steps needed for medical practices to take after being credentialed to maximize the chances of receiving reimbursement. The next critical steps after getting credentialed are (1) to conduct eligibility checks for patient visits and (2) get […]
The average health system saw 110,000 claim denials due to prior authorization and other factors in 2022, a recent study says. KEY TAKEAWAYS: Revenue cycle leaders are placing denials management at the top of the list of areas to improve for 2023. Denials rose to 11% of all claims last year, up nearly 8% from […]
A recent survey highlighted how payment cuts are affecting denial strategies. Healthcare organizations are on the verge of stepping up their denials management strategies in 2023 as rate cuts are expected to impact revenue. On the delivery side, most practices plan to continue their telehealth operations in the New Year, according to the 2023 Part […]
Federal healthcare leaders say they are committed to helping physicians, patients, and health insurance companies by improving the prior authorization process for medical care. On Jan. 17, Center for Medicare & Medicaid Services Administrator and U.S. Surgeon General Vice Admiral, held a listening session with health care stakeholders. That was followed by a conference call […]
The billing and collection process in medical offices can be a time-consuming and error-prone process. This can lead to denied claims, uncollected revenue, and frustrated patients. Medical billing companies are looking for ways to optimize this process to improve efficiency, accuracy, and patient satisfaction. One way to optimize the billing and collection process is to […]