Healthcare organizations rely heavily on accurate coding to ensure timely reimbursement. While CPT and ICD-10 codes often receive most of the attention, HCPCS Level II codes play an equally critical role in billing for supplies, medications, durable medical equipment (DME), ambulance services, and other non-physician services. Even small HCPCS mistakes can trigger claim rejections, payment delays, audits, or compliance risks.
For billing teams already managing rising payer scrutiny and evolving regulations, repeated denials caused by HCPCS coding errors can quickly impact cash flow. Understanding where these errors occur—and how to prevent them—is essential for maintaining a healthy revenue cycle.
Let’s explore the most frequent HCPCS coding mistakes, why they happen, and practical steps your team can take to avoid them.
Why HCPCS Accuracy Matters More Than Ever
HCPCS codes are often tied directly to reimbursement policies, fee schedules, and payer-specific rules. Unlike some CPT services, many HCPCS codes require:
- Strict documentation
- Proper modifiers
- Units of service accuracy
- Medical necessity validation
If even one element is missing or incorrect, payers may deny the entire claim.
Common denial reasons linked to HCPCS include:
- Invalid or outdated code
- Missing modifier
- Incorrect units
- Insufficient documentation
- Medical necessity mismatch
The good news? Most of these issues are preventable with strong processes and proactive checks.
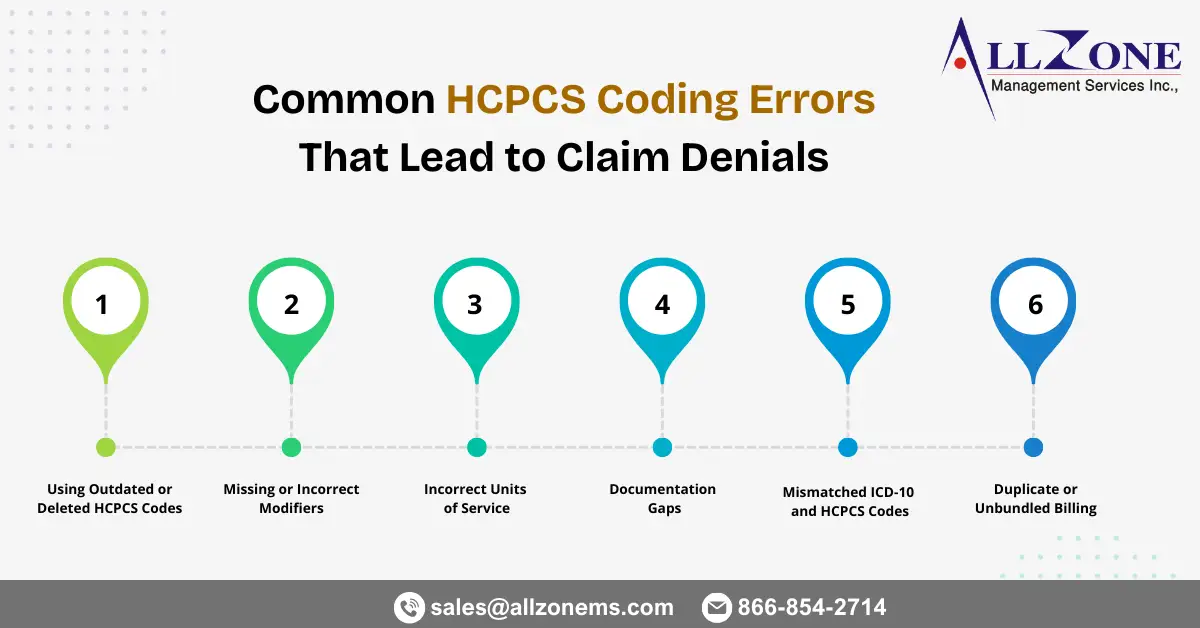
Frequent HCPCS Coding Errors That Cause Denials
1. Using Outdated or Deleted HCPCS Codes
HCPCS codes are updated annually. New drugs, devices, and supplies are added, while older codes may be revised or deleted. When billing teams continue using outdated codes, claims are automatically rejected.
Why this happens:
- Delay in updating charge masters
- Legacy templates in EHR systems
- Lack of staff training on code updates
How to avoid it:
- Update HCPCS files quarterly (not just annually)
- Cross-check payer bulletins regularly
- Audit frequently used codes
Staying current with code sets reduces unnecessary technical denials.
2. Missing or Incorrect Modifiers
Modifiers are critical for HCPCS claims because they explain special circumstances related to supplies or services. Missing modifiers often lead to immediate rejection.
Common examples include:
- NU – New equipment
- RR – Rental equipment
- LT/RT – Laterality
- JW/JZ – Drug wastage reporting
- GA/GY/GZ – Liability or non-covered services
Typical mistakes:
- Forgetting modifiers
- Using the wrong combination
- Applying outdated modifier rules
How to avoid it:
- Build modifier prompts into billing software
- Create specialty-specific cheat sheets
- Train staff on payer-specific requirements
Modifiers are small but powerful. One missing character can mean a denied claim.
3. Incorrect Units of Service
Many HCPCS drug and supply codes are unit-based. Billing incorrect units leads to underpayment or denial.
For example:
- Billing per vial instead of per mg
- Incorrect conversion calculations
- Duplicate unit reporting
Common causes:
- Confusion about package size vs. dosage
- Manual calculations
- Lack of documentation clarity
Prevention strategies:
- Standardize unit conversion charts
- Automate calculations in your system
- Verify documentation before submission
Accurate units ensure correct reimbursement and reduce audit risks.
4. Documentation Gaps
Even when the correct HCPCS code is used, claims may be denied if documentation doesn’t justify the service.
Missing details often include:
- Medical necessity
- Physician order
- Start and stop times
- Supply usage
- Wastage documentation
Payers need proof that the item or service was required and provided.
How to prevent gaps:
- Use documentation templates
- Educate providers on coding requirements
- Conduct pre-bill audits
Better documentation equals stronger claim defensibility.
5. Mismatched ICD-10 and HCPCS Codes
Diagnosis codes must support the medical necessity of HCPCS services. If the diagnosis doesn’t align, payers may deny the claim.
For instance:
- Billing DME without a qualifying diagnosis
- Drug therapy without clinical justification
Prevention tips:
- Use medical necessity edits
- Enable coding software alerts
- Review payer coverage policies
Linking the right diagnosis to the correct HCPCS code improves clean claim rates.
6. Duplicate or Unbundled Billing
Sometimes supplies or services are bundled into other procedures. Billing them separately can trigger denials.
Examples:
- Supplies included in surgical packages
- Bundled drug administration services
How to avoid:
- Understand NCCI edits
- Review bundling rules
- Use compliance tools
Proper bundling ensures compliance and reduces audit exposure.
Practical Prevention Strategies for Billing Teams
Reducing HCPCS coding errors requires more than reactive fixes. It demands proactive planning and continuous improvement.
Strengthen Staff Training
Regular coding workshops help staff stay updated on:
- Code revisions
- Modifier usage
- Payer policies
- Documentation standards
Implement Pre-Bill Audits
A quick quality check before submission catches:
- Missing modifiers
- Invalid codes
- Unit discrepancies
This step alone can significantly improve first-pass acceptance rates.
Leverage Automation
Modern billing systems can:
- Flag outdated codes
- Suggest modifiers
- Validate units
- Check medical necessity
Automation reduces manual errors and boosts efficiency.
Track Denial Trends
Analyze denial reports monthly. Identify:
- Frequent HCPCS issues
- Repeat payer rejections
- High-risk departments
Use data to target training and process improvements.
How Allzone Helps Prevent HCPCS Claim Denials
Managing HCPCS accuracy internally can be time-consuming, especially with limited staff and increasing complexity. This is where partnering with an experienced revenue cycle team makes a difference.
Allzone provides specialized medical billing services that help healthcare organizations:
- Stay updated with the latest HCPCS changes
- Apply correct modifiers and units
- Improve documentation compliance
- Conduct proactive audits
- Reduce denial rates
- Increase clean claim submissions
By combining experienced coders with advanced technology, Allzone helps providers minimize errors and maximize reimbursement.
Final Thoughts
HCPCS coding errors may seem minor, but they can create major revenue disruptions. Missing modifiers, outdated codes, documentation gaps, and incorrect units are among the most common—and preventable—causes of claim denials.
The key is adopting a proactive approach: train your team, update systems regularly, audit claims, and leverage expert support when needed. With the right processes in place, billing teams can reduce denials, accelerate payments, and protect financial stability.
Accurate HCPCS coding isn’t just about compliance—it’s about sustaining your organization’s revenue and delivering uninterrupted patient care.