Introduction to HCPCS R Codes in Radiology Billing Diagnostic radiology services are a cornerstone of modern healthcare, helping physicians diagnose conditions early and create effective treatment plans using imaging technologies such as X-rays, CT scans, MRI, PET scans, and ultrasound. While these procedures improve patient outcomes, the billing and coding process behind them is often […]
Key Takeaways N286 occurs due to missing or incorrect referring provider information Always verify NPI accuracy and payer enrollment Implement front-end checks to prevent denials Automate claim edits for compliance Track and analyze denial trends Partnering with experienced RCM services improves reimbursement rates Claim denials remain one of the biggest challenges in medical billing and […]
Accurate diagnosis coding is the foundation of successful medical billing, clean claims submission, and optimal reimbursement. One of the most frequently used diagnostic chapters in ICD-10-CM is M00–M99: Diseases of the Musculoskeletal System and Connective Tissue. These codes are widely applied across orthopedics, rheumatology, physical therapy, pain management, and primary care. From chronic inflammatory disorders […]
Endovascular procedures have transformed vascular care by offering minimally invasive solutions for conditions such as peripheral artery disease (PAD), aneurysms, and arterial blockages. While these procedures improve patient outcomes and reduce recovery times, they also introduce a new level of complexity in medical billing. For healthcare providers and billing teams, endovascular CPT codes can be […]
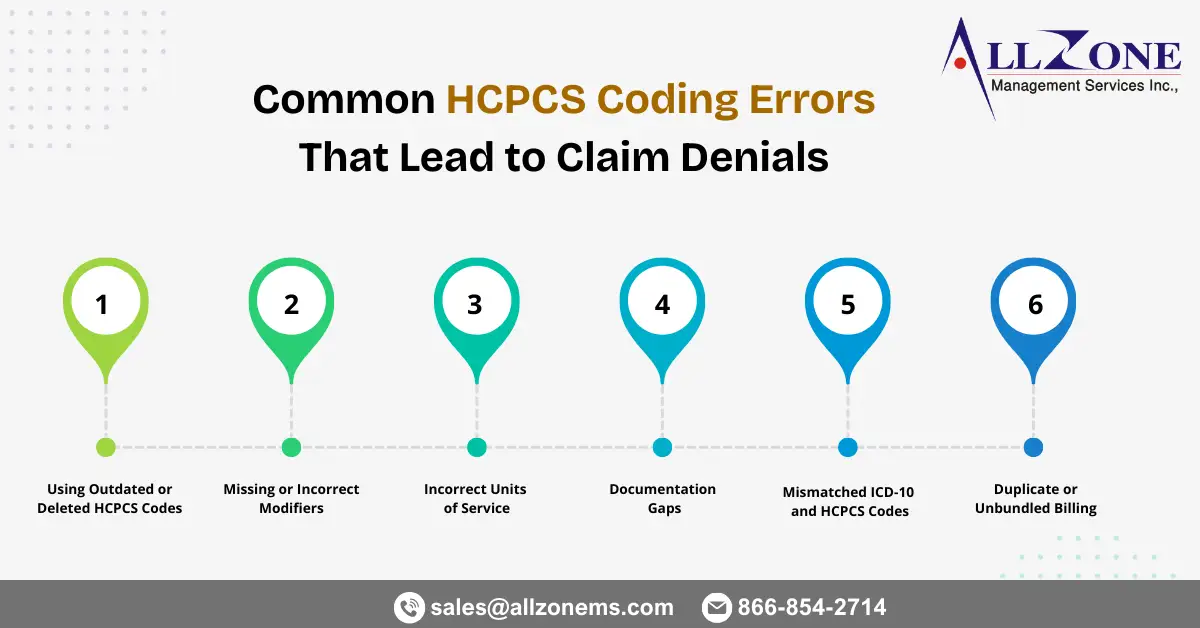
Healthcare organizations rely heavily on accurate coding to ensure timely reimbursement. While CPT and ICD-10 codes often receive most of the attention, HCPCS Level II codes play an equally critical role in billing for supplies, medications, durable medical equipment (DME), ambulance services, and other non-physician services. Even small HCPCS mistakes can trigger claim rejections, payment […]
Maternal healthcare services require some of the most precise and sensitive medical documentation in the healthcare system. From the first prenatal visit to delivery and postpartum recovery, every stage involves detailed clinical reporting and strict compliance with payer guidelines. This is where ICD O00–O9A: Pregnancy, Childbirth & Puerperium codes play a critical role. Accurate coding […]
Dermatology practices handle a wide range of services every day—from routine skin exams and biopsies to complex surgical excisions and cosmetic procedures. While clinical care may appear straightforward, dermatology medical billing can quickly become complicated due to bundled services, lesion counting rules, modifier requirements, and payer-specific edits. Even small coding errors often lead to claim […]
Introduction Accurate ICD-10 ear disorder coding is essential for healthcare providers, ENT specialists, pediatric clinics, and revenue cycle teams that depend on clean claims and timely reimbursements. Ear-related infections and inflammatory conditions are among the most frequently diagnosed problems in outpatient and specialty practices. Without precise coding, even routine ear infection claims can result in […]
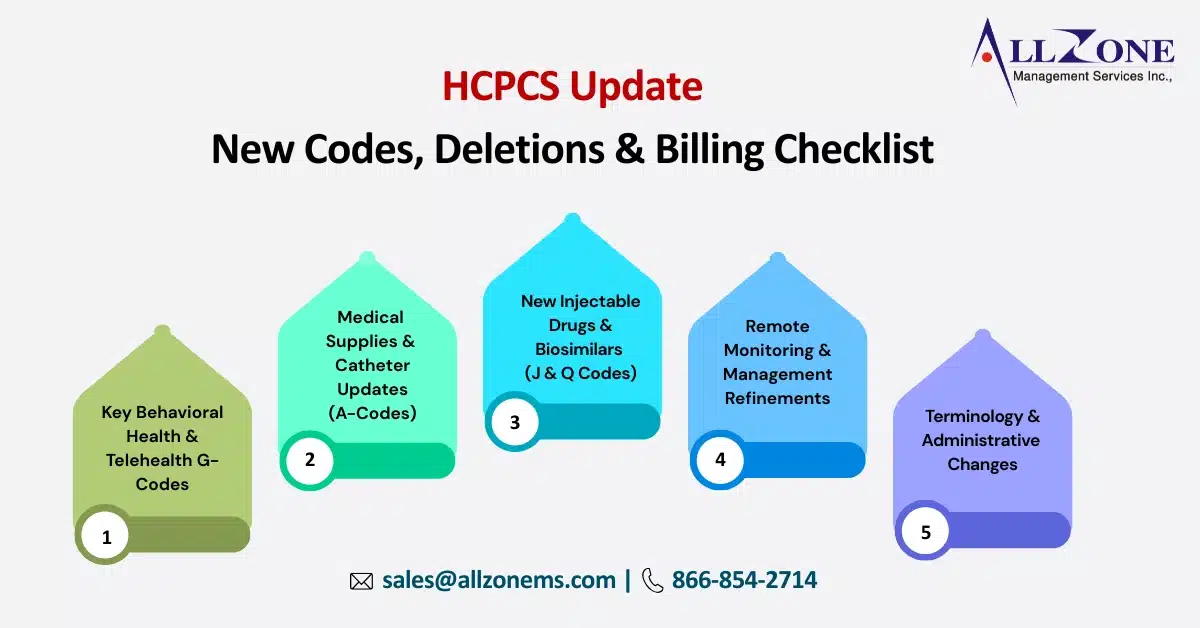
HCPCS Level II & CMS Guidelines HCPCS January 2026 Update: Includes 160 new codes and 101 deletions. Notable additions include new J-codes for FDA-approved products and M-codes for telehealth-conducted encounters. CMS Terminology Shift: CMS is beginning to phase out the term “Social Determinants of Health” in favor of “upstream drivers” in certain official descriptors. NCCI […]
Accurate CPT coding plays a critical role in ensuring timely claim approvals and consistent revenue for healthcare providers. CPT codes communicate the services rendered to payers, and even small errors can result in claim rejections, delayed reimbursements, or compliance risks. As payer rules become stricter and automated claim reviews more common, preventing CPT coding errors […]