Healthcare providers face mounting financial pressures due to rising operational costs, evolving regulatory requirements, and shrinking reimbursement rates. One of the most critical areas affecting revenue cycle efficiency is claims denial management. Despite advancements in technology, many healthcare organizations still rely on manual claims denial management, leading to inefficiencies, revenue leakage, and administrative burdens. This […]
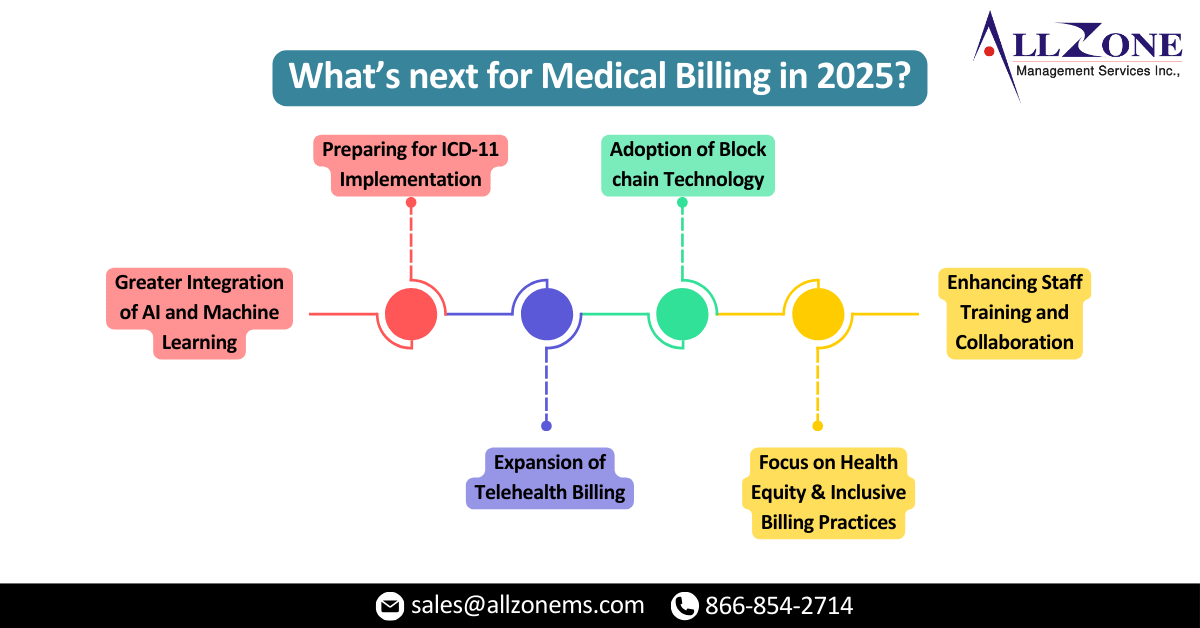
The medical billing landscape is evolving rapidly, driven by advancements in technology, regulatory updates, and shifting patient expectations. Staying informed about Top Medical Billing Trends is crucial. As we enter 2025, healthcare providers and medical billing companies must stay ahead of the curve to ensure compliance, maximize revenue, and improve patient satisfaction. This newsletter will […]
Claim denials are a significant headache for healthcare providers, impacting revenue and administrative efficiency. While denials can stem from various issues, a large majority are rooted in documentation errors, particularly those related to demonstrating medical necessity. Defining Medical Necessity: The American Medical Association (AMA) defines medical necessity as healthcare services or products provided to a […]
In the ever-evolving field of medical billing, denied claims remain a significant obstacle for healthcare providers. Studies reveal that over 10% of claims face initial rejection by insurers, leading to revenue losses, administrative strain, and frustration for all stakeholders. To mitigate these challenges and ensure financial stability, an effective denial management process is essential. However, […]
Medical coding denials are a common challenge for healthcare providers and revenue cycle management (RCM) teams. They can disrupt cash flow, delay reimbursements, and increase administrative workloads. Avoiding these denials requires a proactive approach that addresses their root causes, ensures compliance with regulations, and fosters a culture of continuous improvement. In this blog, we’ll explore […]
As 2024 draws to a close, the healthcare industry reflects on a year of groundbreaking innovations, policy shifts, and evolving challenges in medical billing. The Allzone Management Services team has seen first-hand how these changes have improved revenue cycle management (RCM), streamlined processes, and patient satisfaction as a result of these changes. In this newsletter, […]
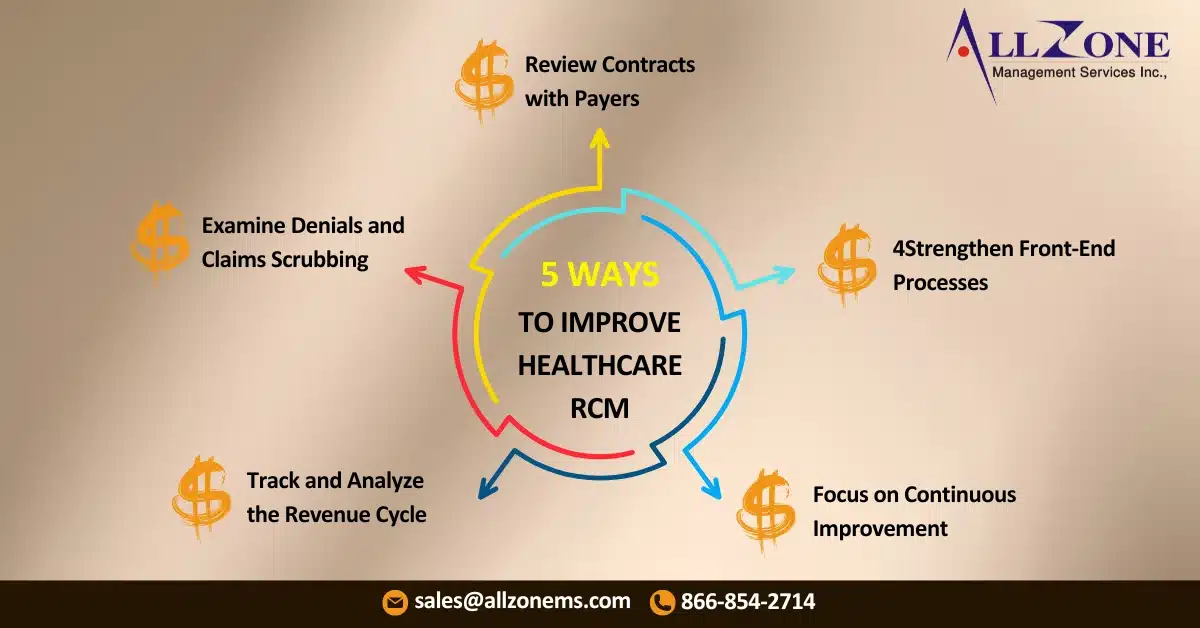
The healthcare industry operates under a unique framework. Unlike traditional businesses where customers pay directly for a product or service, healthcare providers navigate a complex system involving multiple players, including payers, claims management, and reimbursements. To Improve Revenue Cycle Management, healthcare providers must understand this intricate system and implement efficient strategies to optimize their revenue […]
Medical billing teams and healthcare providers need to ensure their revenue cycle management processes are ready for the New Year as 2024 draws to a close. In order to succeed in 2025, a proactive, well-organized approach is essential. In order to help you maintain compliance, improve financial outcomes, and set the stage for success in […]
Chronic Care Management codes are increasingly being adopted by healthcare providers to address care fragmentation for patients with multiple chronic conditions. However, a recent study published in the American Academy of Family Physicians suggests that while CCM is gaining traction, challenges persist in its implementation and reimbursement. A Growing Trend The study, which analyzed Medicare […]
Claim denials continue to pose a significant challenge to healthcare claims management. Recent surveys indicate a substantial increase in denial rates, with many providers experiencing denial rates exceeding 10%. This issue has far-reaching consequences, impacting operational efficiency, financial stability, and ultimately, patient care The High Cost of Denials Healthcare providers face substantial financial losses due […]